June 13, 2025
Coronary artery disease affects millions of Americans, with many requiring medical interventions to restore blood flow to the heart. Heart treatments have evolved significantly, offering various options for patients.
Two common procedures for treating coronary artery disease are often considered: minimally invasive treatments and more invasive surgical options. Understanding the differences between these procedures is crucial for patients and healthcare providers to make informed decisions.
This article aims to provide a comprehensive comparison, helping readers understand the key aspects of each treatment option.
Key Takeaways
- Overview of coronary artery disease and its impact
- Comparison of treatment options for heart disease
- Key differences between minimally invasive and surgical procedures
- Factors to consider when choosing a treatment plan
- Importance of informed decision-making in heart care
Understanding Coronary Artery Disease
Understanding coronary artery disease is crucial for grasping the reasons behind heart-related conditions and the need for interventions like angioplasty and bypass surgery. Coronary artery disease occurs when the coronary arteries, the major blood vessels that supply blood to the heart, become damaged or diseased.
How Plaque Affects Your Heart
Plaque buildup in the coronary arteries can lead to their narrowing or blockage, a condition known as atherosclerosis. This restricts blood flow to the heart muscle, potentially causing chest pain (angina), shortness of breath, or other symptoms. Over time, severe plaque buildup can lead to a heart attack if the blood flow is completely blocked.
When Intervention Becomes Necessary
When coronary artery disease advances, medical intervention becomes necessary to restore blood flow to the heart. This can involve procedures like angioplasty, where a blocked artery is opened, or coronary artery bypass grafting (CABG), where a graft is used to bypass the blocked section of the artery. The choice between these procedures depends on the extent and location of the disease.
| Disease Stage | Symptoms | Intervention |
|---|---|---|
| Mild Plaque Buildup | Minimal or no symptoms | Lifestyle changes, medication |
| Moderate to Severe | Angina, shortness of breath | Angioplasty or CABG |
| Severe Blockage | Heart attack | Emergency angioplasty or CABG |
Angioplasty vs. Bypass Surgery: What's the Difference?
Understanding the differences between angioplasty and bypass surgery is crucial for patients facing coronary artery disease treatment decisions. Both procedures aim to restore blood flow to the heart, but they differ significantly in their approach and application.
Basic Definitions and Purposes
Angioplasty is a minimally invasive procedure where a catheter is used to inflate a balloon that opens up the blocked artery. Often, a stent is placed to keep the artery open. Angioplasty is primarily used to treat coronary artery disease by improving blood flow to the heart.
Bypass surgery, on the other hand, involves surgically grafting a vessel to bypass the blocked section of the coronary artery, thereby rerouting blood flow around the blockage. This procedure is often recommended for patients with complex or multiple blockages.
Key Differences at a Glance
The key differences between angioplasty and bypass surgery can be summarized as follows:
- Invasiveness: Angioplasty is less invasive compared to bypass surgery, which requires open-heart surgery.
- Recovery Time: Angioplasty typically has a shorter recovery time than bypass surgery.
- Blockage Complexity: Angioplasty is often used for simpler blockages, while bypass surgery is preferred for more complex or multiple blockages.
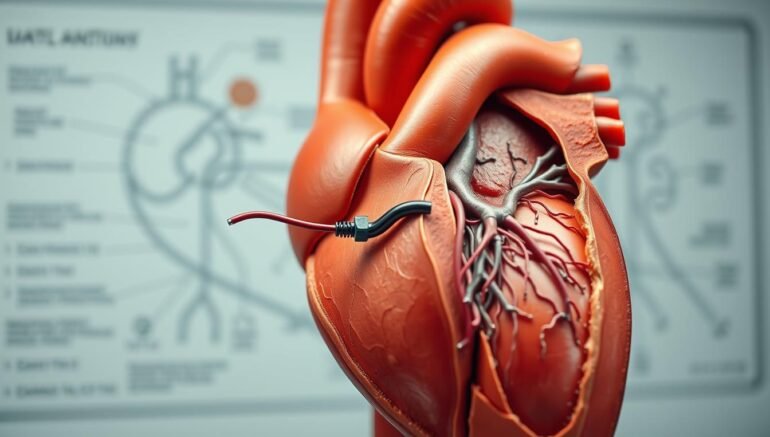
Angioplasty Explained in Detail
Understanding angioplasty is crucial for patients considering treatment options for heart disease. Angioplasty, also known as percutaneous transluminal angioplasty (PTA), is a minimally invasive procedure used to widen narrowed or obstructed arteries or veins. This procedure is typically performed to relieve symptoms associated with coronary artery disease.
The Procedure Step by Step
The angioplasty procedure involves several key steps. First, the patient is given local anesthesia to numb the area where the catheter will be inserted, typically in the groin or arm. A catheter with a balloon tip is then guided through the blood vessels to the blocked artery. Once in position, the balloon is inflated to push aside the plaque and stretch the artery, improving blood flow. The balloon is then deflated and removed.
Key steps in the angioplasty procedure:
- Insertion of the catheter
- Guiding the catheter to the blocked artery
- Inflating the balloon to widen the artery
- Deflating and removing the balloon
Types of Stents Used
Often, a stent is placed during angioplasty to keep the artery open. There are different types of stents used, each with its own characteristics.
Bare-Metal Stents
Bare-metal stents are made of metal mesh and provide structural support to keep the artery open. While effective, they have a higher risk of causing the artery to narrow again over time.
Drug-Eluting Stents
Drug-eluting stents are coated with medication that helps prevent the artery from becoming blocked again. These stents have been shown to reduce the risk of restenosis compared to bare-metal stents.
Angioplasty Without Stents
In some cases, angioplasty can be performed without the placement of a stent. This approach is often used for smaller blockages or in situations where the risk of complications with stenting is considered high. However, the risk of the artery becoming blocked again is higher without a stent.
The decision to use a stent or not depends on various factors, including the patient’s overall health, the location and severity of the blockage, and the specific characteristics of the plaque.
Coronary Bypass Surgery Explained
Bypass surgery, or coronary artery bypass grafting (CABG), is a surgical procedure used to improve blood flow to the heart. This operation is typically recommended for patients with severe coronary artery disease, where the arteries supplying blood to the heart are blocked or severely narrowed.
The Surgical Process
The surgical process of coronary bypass surgery involves several key steps. First, the patient is given general anesthesia to ensure they remain pain-free and asleep during the procedure. The surgeon then makes an incision in the chest, often cutting through the sternum to access the heart. The patient is connected to a heart-lung machine, which takes over the function of the heart and lungs during the surgery.
The surgeon then harvests a graft – a blood vessel taken from another part of the body – to bypass the blocked artery. Once the graft is attached, it provides a new pathway for blood to flow to the heart muscle, effectively bypassing the blockage.
Types of Bypass Grafts
There are different types of grafts used in coronary bypass surgery, each with its own advantages.
Saphenous Vein Grafts
Saphenous vein grafts are taken from the leg. They are commonly used because they are readily available and of suitable length. However, they may have a higher risk of occlusion over time compared to arterial grafts.
Arterial Grafts
Arterial grafts, taken from arteries in the chest or arm, are preferred for their durability and long-term patency. The left internal mammary artery (LIMA) is frequently used due to its excellent long-term results.
| Graft Type | Source | Long-term Patency |
|---|---|---|
| Saphenous Vein Grafts | Leg | Lower |
| Arterial Grafts | Chest or Arm | Higher |
Minimally Invasive Options
Minimally invasive coronary bypass surgery is an alternative to traditional CABG. This approach involves smaller incisions and may reduce recovery time. Techniques such as off-pump CABG, where the surgery is performed without connecting the patient to a heart-lung machine, are also being used more frequently.
According to a study published in the Journal of Thoracic and Cardiovascular Surgery, “Minimally invasive CABG can reduce morbidity and shorten hospital stay.” This highlights the potential benefits of less invasive surgical techniques in coronary bypass surgery.
When Is Angioplasty Recommended?
For individuals with specific heart conditions, angioplasty may be the preferred treatment method. This procedure is often considered for patients who have coronary artery disease and are experiencing symptoms such as chest pain or shortness of breath.
Ideal Candidates
Ideal candidates for angioplasty are typically those with blockages in one or two major coronary arteries. Patients who have had a heart attack or are at risk of having one may also be considered for this procedure. Additionally, individuals who have not responded well to medication or other treatments may benefit from angioplasty.
The decision to recommend angioplasty is based on various factors, including the severity of the blockage, the overall health of the patient, and the presence of other medical conditions.
Limitations and Contraindications
While angioplasty is a valuable treatment option, it is not suitable for everyone. Limitations include the presence of complex coronary artery disease or multiple blockages, which may make the procedure more challenging. Contraindications may include severe kidney disease, bleeding disorders, or other conditions that could complicate the procedure.
Understanding these factors is crucial in determining whether angioplasty is the right treatment choice for a patient.
When Is Bypass Surgery Recommended?
Coronary artery bypass grafting (CABG), commonly known as bypass surgery, is a surgical procedure that can significantly improve heart health in certain cases. This operation involves grafting a healthy blood vessel onto a blocked or narrowed coronary artery, thereby bypassing the obstruction and restoring blood flow to the heart muscle.
Ideal Candidates
Bypass surgery is typically recommended for patients with complex coronary artery disease, particularly those with multiple blockages or blockages that are not easily treatable with angioplasty. Ideal candidates include individuals with significant blockages in multiple coronary arteries, those with diabetes, and patients whose blockages are located in critical areas or are too severe for angioplasty.
Additionally, patients who have not responded well to other treatments or have recurrent symptoms after angioplasty may be considered for bypass surgery. The decision is often made after a thorough evaluation, including coronary angiography and other diagnostic tests, to assess the extent and severity of the disease.
Limitations and Contraindications
While bypass surgery can be lifesaving, it is not suitable for everyone. Contraindications include severe lung disease, certain heart conditions, and other comorbidities that may increase surgical risks. Advanced age is not an absolute contraindication, but older patients are typically assessed on a case-by-case basis, considering their overall health and potential for recovery.
Furthermore, the presence of significant comorbid conditions, such as severe kidney disease or frailty, may limit the suitability of bypass surgery. The surgical team evaluates each patient’s risk factors and overall health to determine the most appropriate treatment plan.
Recovery and Rehabilitation
The journey to recovery after angioplasty or bypass surgery involves several key steps and considerations. Understanding the recovery process is essential for patients to manage their expectations and make necessary lifestyle adjustments.
Angioplasty Recovery Timeline
Recovery from angioplasty is generally quicker compared to bypass surgery. Most patients can resume normal activities within a few days to a week after the procedure. The angioplasty recovery timeline typically involves:
- Immediate post-procedure monitoring
- Discharge from the hospital within 24 hours
- Rest and limited activity for a few days
- Gradual return to normal activities
Bypass Surgery Recovery Timeline
Bypass surgery requires a longer recovery period. Patients typically spend several days in the hospital and may need several weeks to recover fully at home. The bypass surgery recovery timeline includes:
- Hospital stay of 5 to 7 days
- Several weeks of rest and recovery at home
- Gradual increase in physical activity as advised by the doctor
- Follow-up appointments to monitor healing
Required Lifestyle Changes After Each Procedure
Regardless of whether a patient undergoes angioplasty or bypass surgery, certain lifestyle changes are crucial for a successful recovery and long-term health. These include:
- Adopting a heart-healthy diet
- Engaging in regular physical activity as recommended
- Quitting smoking
- Managing stress
- Adhering to prescribed medication regimens
By making these adjustments, patients can improve their overall health outcomes and reduce the risk of future cardiovascular issues.
Risks and Complications
When considering angioplasty or bypass surgery, it’s essential to understand the potential risks and complications associated with each procedure. Both are effective treatments for coronary artery disease, but they come with their own set of risks.
Potential Complications of Angioplasty
Angioplasty, while generally considered safe, carries certain risks. Understanding these risks is crucial for patients to make informed decisions about their treatment.
Short-Term Risks
Short-term risks associated with angioplasty include bleeding at the catheter site, bruising, and damage to the blood vessels. There’s also a risk of allergic reactions to the dye used during the procedure. In rare cases, angioplasty can cause heart attack or stroke.
Long-Term Risks
Long-term risks of angioplasty include restenosis, or the re-narrowing of the arteries, which can occur in some patients. There’s also a risk of stent thrombosis, a condition where a blood clot forms inside the stent.
Potential Complications of Bypass Surgery
Bypass surgery, like angioplasty, comes with its own set of potential complications. Understanding these risks is vital for patients to make informed decisions.
Short-Term Risks
Short-term risks of bypass surgery include infection, bleeding, and adverse reactions to anesthesia. Patients are also at risk for heart attack, stroke, or kidney failure during or after the surgery.
Long-Term Risks
Long-term risks associated with bypass surgery include graft failure, where the grafted vessel becomes blocked, and return of angina symptoms. Some patients may also experience cognitive dysfunction after the surgery.
Understanding these risks and complications is crucial for patients and healthcare providers to make informed decisions about the most appropriate treatment for coronary artery disease.
Long-Term Outcomes and Success Rates
Understanding the long-term outcomes of angioplasty and bypass surgery is crucial for patients and healthcare providers alike. These procedures, used to treat coronary artery disease, have different success rates and long-term results.
Angioplasty Long-Term Results
Angioplasty, a minimally invasive procedure, has shown promising long-term results. Studies indicate that patients who undergo angioplasty have a significant reduction in symptoms and improvement in quality of life. However, the success rate can be influenced by factors such as the type of stent used and patient compliance with post-procedure medication.
Key statistics: A study published in the Journal of the American College of Cardiology found that the 5-year survival rate for patients after angioplasty was approximately 85%.
Bypass Surgery Long-Term Results
Bypass surgery, on the other hand, involves grafting a healthy vessel to bypass blocked coronary arteries. Long-term results for bypass surgery have shown durability, with many patients experiencing relief from symptoms for years after the procedure.
Notably, a study in the New England Journal of Medicine highlighted that the 10-year survival rate for patients post-bypass surgery was around 75%, with significant variation based on graft type and patient health.
Comparative Studies and Statistics
Comparative studies between angioplasty and bypass surgery have provided valuable insights. A meta-analysis published in the Lancet compared outcomes of both procedures and found that while both are effective, bypass surgery often results in fewer repeat procedures.
“The choice between angioplasty and bypass surgery should be tailored to the individual patient, considering factors such as the extent of coronary disease and patient comorbidities.”
Decision-Making Factors: How Doctors Choose
The decision between angioplasty and bypass surgery is complex and depends on various medical and patient-specific factors. Doctors must weigh these elements carefully to determine the most appropriate treatment for each patient.
Medical Considerations
Medical considerations play a crucial role in the decision-making process. These include the severity of coronary artery disease, the location and number of blockages, and the patient’s overall heart health. Doctors assess the extent of the disease through diagnostic tests like angiograms to understand the complexity of the blockages.
Patient-Specific Factors
Patient-specific factors are equally important. These factors include the patient’s age, overall health, medical history, and lifestyle. For instance, patients with diabetes or those who have had previous heart surgeries may require a different approach.
| Factor | Angioplasty | Bypass Surgery |
|---|---|---|
| Severity of Disease | Suitable for less complex cases | Preferred for more complex, multi-vessel disease |
| Patient Age | Often considered for older patients or those with higher surgical risks | May be recommended for younger patients to provide a more durable solution |
By considering both medical and patient-specific factors, doctors can make an informed decision that best suits the patient’s needs.
Conclusion
Understanding the differences between angioplasty and bypass surgery is crucial for making informed decisions about heart health. Both procedures aim to restore blood flow to the heart, but they vary significantly in terms of approach, benefits, and risks.
Angioplasty is a minimally invasive procedure that involves using a balloon to widen narrowed arteries. It is often used in conjunction with stenting to keep the artery open. Bypass surgery, on the other hand, involves surgically grafting a vessel to bypass the blocked section of the artery.
The choice between angioplasty and bypass surgery depends on various factors, including the severity of coronary artery disease, overall health, and medical history. By understanding the key differences between these procedures, patients can better navigate their treatment options and make decisions that align with their health goals.
In conclusion, both angioplasty and bypass surgery play critical roles in managing heart health. By considering individual circumstances and medical recommendations, patients can make informed choices that improve their cardiovascular well-being.
FAQ
What is the main difference between angioplasty and bypass surgery?
Angioplasty is a minimally invasive procedure that uses a balloon to widen narrowed or blocked coronary arteries, often with the placement of a stent. Bypass surgery, on the other hand, involves surgically grafting a vessel to bypass the blocked section of the artery.
How do I know if I’m a candidate for angioplasty or bypass surgery?
The choice between angioplasty and bypass surgery depends on several factors, including the severity and location of your coronary artery disease, your overall health, and your medical history. Your doctor will assess these factors to recommend the most suitable procedure.
What are the risks associated with angioplasty and bypass surgery?
Both procedures carry risks, including bleeding, infection, and reaction to anesthesia. Angioplasty risks include stroke and coronary artery damage, while bypass surgery risks include graft failure and heart attack. Your doctor will discuss the specific risks relevant to your situation.
How long does recovery take after angioplasty and bypass surgery?
Recovery time varies. Angioplasty typically has a shorter recovery period, often within a few days to a week, whereas bypass surgery may require several weeks to a few months for full recovery. Lifestyle changes are crucial for a successful recovery in both cases.
Can I undergo angioplasty or bypass surgery if I have other health conditions?
The presence of other health conditions can affect your eligibility for these procedures. Your doctor will evaluate your overall health, including conditions like diabetes, kidney disease, or previous heart conditions, to determine the best course of treatment.
What lifestyle changes are necessary after undergoing angioplasty or bypass surgery?
After either procedure, it’s essential to adopt a heart-healthy lifestyle, including a balanced diet, regular exercise, quitting smoking, and managing stress. Your healthcare provider may also recommend specific medications to manage cholesterol, blood pressure, or other conditions.
Are there any long-term outcomes or success rates for angioplasty and bypass surgery?
Both procedures have been shown to be effective in treating coronary artery disease. Long-term success rates vary based on factors like the severity of disease, overall health, and adherence to post-procedure lifestyle recommendations. Studies have compared outcomes, providing insights into the effectiveness of each procedure.
How do doctors decide between recommending angioplasty or bypass surgery?
Doctors consider medical factors, such as the extent and location of coronary artery disease, as well as patient-specific factors, including overall health, preferences, and lifestyle. This comprehensive assessment guides the decision-making process to choose the most appropriate treatment.






