
May 10, 2025
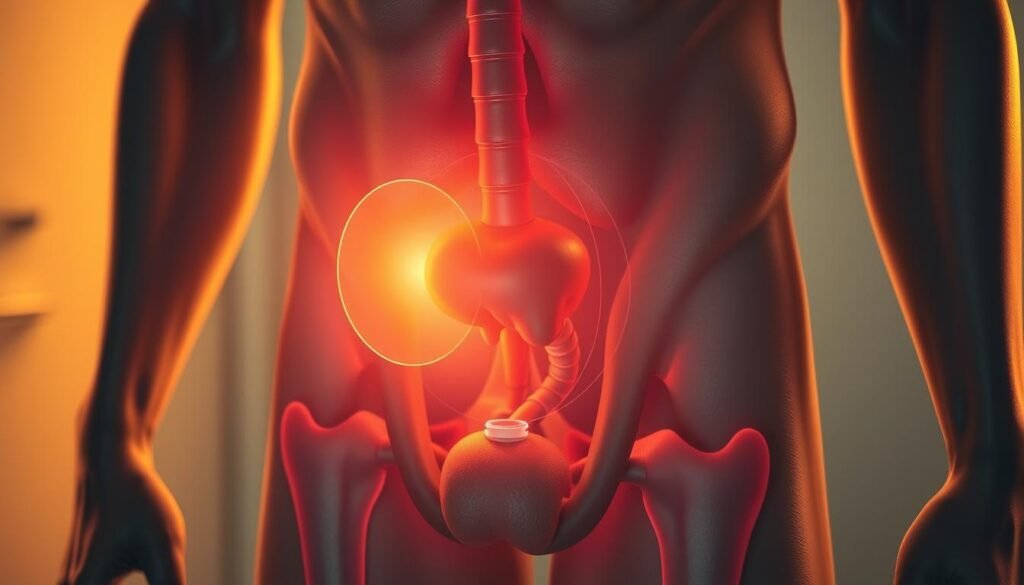
Did you know millions of men in the U.S. have prostatitis? This is when the prostate gland gets inflamed. It can cause pain and trouble with urination.
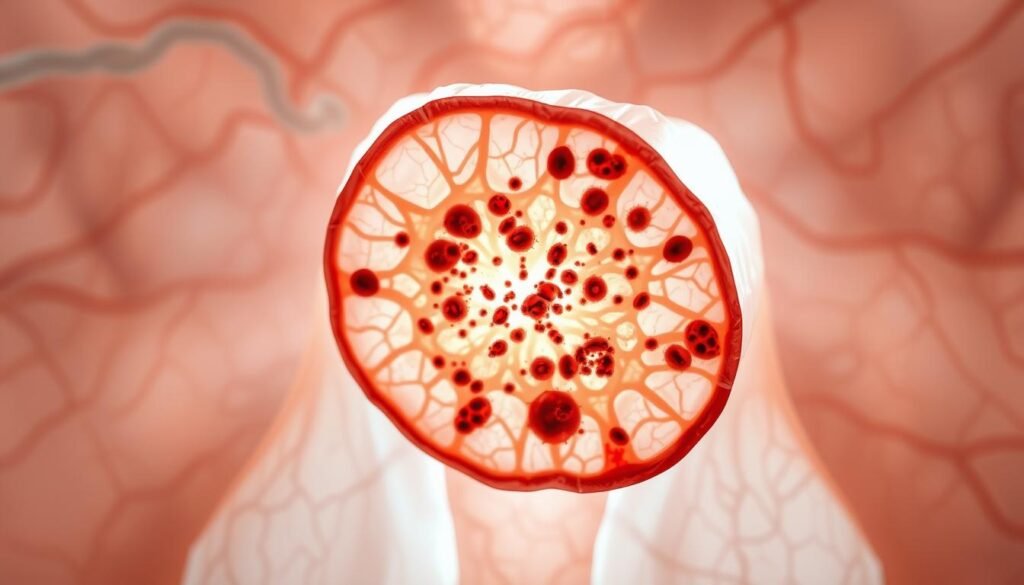
The prostate gland is key for men’s health. It makes fluid that helps sperm cells grow.
When the gland gets inflamed, symptoms can appear. Prostatitis awareness is important. It shows how STIs can be linked to it, making it vital to know the causes and effects.
Key Takeaways
- Prostatitis is a common condition affecting millions of men.
- The prostate gland is vital for the male reproductive system.
- Inflammation of the prostate can lead to discomfort and urinary issues.
- STIs can be a significant factor in prostatitis cases.
- Raising prostatitis awareness is essential for early diagnosis and treatment.
Understanding Prostatitis: Causes and Symptoms
Men who suffer from prostatitis know how it can ruin their life. It’s when the prostate gland gets inflamed. This can happen for many reasons.
What is Prostatitis?
Prostatitis makes the prostate gland swell and get irritated. It can be from infections, injuries, or other health issues. Bacterial infections are a big cause, like UTIs or STIs.
Common Symptoms of Prostatitis
Symptoms of prostatitis include pain in the pelvic area and trouble urinating. Some people also get a fever. Chronic prostatitis can cause ongoing pain.
Types of Prostatitis
Prostatitis is divided into types based on its causes and how long it lasts.
Acute Bacterial Prostatitis
This is a sudden infection of the prostate, usually from bacteria.
Chronic Bacterial Prostatitis
This is a long-lasting infection that keeps coming back, needing long-term treatment.
Chronic Pelvic Pain Syndrome
This is the most common type. It’s chronic pain in the pelvic area without an infection.
| Type of Prostatitis | Causes | Common Symptoms |
|---|---|---|
| Acute Bacterial Prostatitis | Bacterial infection | Sudden pain, fever, urinary issues |
| Chronic Bacterial Prostatitis | Recurring bacterial infection | Recurring pain, urinary discomfort |
| Chronic Pelvic Pain Syndrome | Unknown, possibly non-bacterial | Chronic pelvic pain, discomfort |
Prostatitis and STIs – The Overlooked Connection
The link between prostatitis and sexually transmitted infections (STIs) is key for men’s health. Studies show that STIs can cause prostate inflammation, known as prostatitis. This inflammation comes from various pathogens, often spread through sex.
How STIs Can Lead to Prostate Inflammation
STIs like chlamydia and gonorrhea can infect the urinary tract. This infection can move up to the prostate gland, causing inflammation. The bacteria irritate the prostate, leading to swelling and pain. Early detection and treatment of STIs are key to avoid these issues.
Statistical Evidence of the Connection
Research has found a strong link between STIs and prostatitis. Men with STI histories are more likely to get chronic prostatitis. Data analysis shows that STIs are a risk factor for prostatitis.
Why This Connection Is Often Missed in Clinical Settings
Despite the evidence, the STI-prostatitis link is often ignored in healthcare. This might be because prostatitis symptoms are not clear-cut. They can look like other conditions, making it hard to diagnose. Healthcare providers need to be aware of this connection for proper diagnosis and treatment.
Common STIs That Can Cause Prostatitis
STIs can cause prostatitis, leading to long-term inflammation of the prostate gland. Knowing which STIs can cause this is key to treating it effectively.
Chlamydia and the Prostate
Chlamydia trachomatis is a common STI linked to prostatitis. It can cause long-term inflammation in the prostate, leading to pain and discomfort when urinating. This shows why testing for STIs is so important in diagnosing prostatitis.
Gonorrhea's Impact on Prostate Health
Gonorrhea, caused by Neisseria gonorrhoeae, can also cause prostatitis. If not treated, it can lead to infertility. This highlights the need for quick treatment of STIs to protect prostate health.
Mycoplasma and Ureaplasma Infections
Mycoplasma and ureaplasma bacteria can cause infections in the urogenital tract, leading to prostatitis. These infections are often spread through sex and can cause long-term prostatitis if not treated. Special tests are needed to diagnose these infections.
Trichomoniasis and Other STIs
Trichomonas vaginalis causes trichomoniasis, an STI linked to prostatitis. Other STIs, like viral infections, can also affect the prostate. Testing for all STIs is important to find the cause of prostatitis.
| STI | Causative Agent | Impact on Prostate Health |
|---|---|---|
| Chlamydia | Chlamydia trachomatis | Chronic inflammation, pelvic pain |
| Gonorrhea | Neisseria gonorrhoeae | Acute or chronic prostatitis, infertility |
| Mycoplasma/Ureaplasma | Mycoplasma/Ureaplasma species | Chronic prostatitis, urogenital infections |
| Trichomoniasis | Trichomonas vaginalis | Prostatitis, urogenital symptoms |
Diagnosis: Identifying STI-Related Prostatitis
Understanding STI-related prostatitis requires a detailed approach. It involves various tests and a full medical check-up.
Diagnostic Tests for Prostatitis
Several tests help find prostatitis. A digital rectal exam (DRE) checks the prostate for tenderness. A urine test looks for infection or inflammation.
A transrectal ultrasound gives a closer look at the prostate. A blood test for prostate-specific antigen (PSA) helps check prostate health.
STI Testing Protocols
For STI-related prostatitis, specific tests are needed. These include urine PCR (Polymerase Chain Reaction) tests and swab tests. They check for pathogens like Chlamydia trachomatis or Neisseria gonorrhoeae.
Differential Diagnosis Challenges
Diagnosing STI-related prostatitis can be tricky. It’s hard to tell it apart from other prostate issues. A detailed medical history and physical exam, along with test results, are key to a correct diagnosis.
When to Seek Medical Attention
If you have symptoms like pelvic pain, painful urination, or fever, see a doctor. Early treatment is important to avoid complications and ease symptoms.
Treatment Approaches for STI-Induced Prostatitis
Treating prostatitis caused by STIs needs a multi-faceted approach. This helps to ease symptoms and get rid of the infection. The treatment plan depends on the cause, how bad the symptoms are, and the patient’s health.
Antibiotic Therapy and Medication Options
Antibiotics are key in treating STI-induced prostatitis. The right antibiotic depends on the pathogen. For example, Chlamydia and Mycoplasma need azithromycin or doxycycline. Gonorrhea might need ceftriaxone and azithromycin together.
Medicines like tamsulosin or alfuzosin can help with urination. They relax muscles around the prostate and bladder.
Managing Chronic Symptoms
It’s important to manage chronic symptoms for better quality of life. This includes pain management, lifestyle changes, and alternative therapies. Regular check-ups with healthcare providers are key to adjusting treatment plans.
Pain Management Strategies
Pain management is vital in treating STI-induced prostatitis. Painkillers can help with physical pain. For severe pain, treatments like pelvic floor physical therapy or nerve blocks might be suggested.
Complementary and Alternative Treatments
Some patients find relief in complementary and alternative treatments. These include dietary changes, herbal supplements, and stress management. These can help with symptoms and improve overall well-being.
| Treatment Approach | Description | Benefits |
|---|---|---|
| Antibiotic Therapy | Targeted antibiotics for the causative STI | Effective in eradicating the infection |
| Pain Management | Painkillers and other pain relief strategies | Reduces discomfort and improves quality of life |
| Complementary Therapies | Dietary changes, herbal supplements, stress management | Enhances overall well-being and symptom management |
Psychological Impact and Quality of Life Considerations
Chronic prostatitis affects a man’s well-being deeply. It goes beyond physical symptoms to touch mental health and relationships. This condition is not just a physical issue but also has big psychological and social effects.
Mental Health Aspects of Chronic Prostatitis
Chronic prostatitis can cause anxiety and depression in men. The ongoing symptoms bring uncertainty and distress. This affects a person’s mental health and quality of life greatly.
As one study found, “The psychological burden of chronic prostatitis can be as debilitating as the physical symptoms.”
Sexual Function and Relationship Challenges
Chronic prostatitis can lead to erectile dysfunction or painful ejaculation. This can put a strain on relationships. It affects not just the person but also their partner.
Open communication and support are key in managing these challenges.
Support Resources for Patients
There are many support resources for men with chronic prostatitis. These include counseling, support groups, and online forums. Raising prostatitis awareness helps reduce stigma and encourages men to seek help.
Understanding the link between prostatitis and STIs is also important. It helps with STI prevention tips and improves health outcomes. By addressing the psychological impact and quality of life, healthcare providers can offer better care.
Conclusion
It’s important to know how prostatitis and STIs are connected. This connection is often missed, leading to long-term suffering and health issues.
Understanding the role of STIs in prostatitis is key. It helps in managing chronic prostatitis better. Healthcare providers can then create more effective treatment plans.
Prostatitis and STIs need a team effort to tackle. By raising awareness, we can improve diagnosis and treatment. This will help those affected live better lives.
FAQ
What is prostatitis, and how is it related to STIs?
Prostatitis is when the prostate gland gets inflamed. This can happen due to certain sexually transmitted infections (STIs). STIs like chlamydia, gonorrhea, and trichomoniasis can cause this inflammation.
What are the common symptoms of prostatitis?
Symptoms of prostatitis include pain in the pelvic area and trouble urinating. You might also feel pain when you ejaculate and have a fever. The symptoms can vary based on the cause and type of prostatitis.
How are STIs diagnosed in relation to prostatitis?
Doctors use a physical exam, medical history, and lab tests to diagnose STIs related to prostatitis. Tests include urine tests, prostate fluid analysis, and STI screening like PCR or culture.
What treatment options are available for STI-induced prostatitis?
Treatment for STI-induced prostatitis usually involves antibiotics to target the STI. You might also need pain management, lifestyle changes, and other therapies to manage symptoms.
Can prostatitis caused by STIs become chronic?
Yes, if not treated properly, STI-induced prostatitis can become chronic. Chronic prostatitis can lead to ongoing pain, discomfort, and sexual problems.
How can chronic prostatitis affect mental health?
Chronic prostatitis can really affect your mental health. It can cause anxiety, depression, and stress due to the ongoing symptoms and how they impact your life and relationships.
What support resources are available for patients with prostatitis?
There are many resources for patients with prostatitis. You can find healthcare providers, support groups, online forums, and counseling services. These help with both the physical and emotional aspects of the condition.
How can prostatitis be prevented?
To prevent prostatitis, practice safe sex and keep your genital area clean. If you notice symptoms of prostatitis or STIs, see a doctor right away.
Are there any alternative treatments for prostatitis?
Yes, alternative treatments include acupuncture, herbal supplements, and making lifestyle changes. But, always talk to a healthcare provider before trying these.
Why is it important to recognize the link between prostatitis and STIs?
It’s key to understand the link between prostatitis and STIs for proper treatment. It shows the importance of STI screening and the right antibiotics to treat the cause.






